Urogenital symptoms during menopause
Some of the most common complaints of women going through the menopause are vaginal and bladder symptoms. Dryness, pain during sex, increased urgency to urinate and general discomfort, can be experienced unfortunately. The vagina, vulval tissue, urethra and lower trigone of the bladder are teeming with oestrogen receptors, hence, when oestrogen declines in menopause, women can experience changes to these tissues.
One of the roles of oestrogen is to maintain the health and vitality of an important layer of the vaginal wall - the vaginal mucosa. In a healthy vagina, this thick layer of cells produces a wide range of important substances, from vaginal mucus, which keeps the vagina moist and lubricated, to glycogen and amino acids which serve as food for healthy, protective bacteria in this environment.
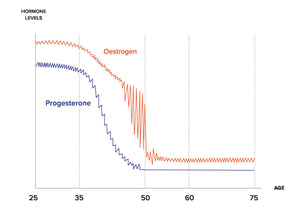
Oestrogen decline
The reduction of oestrogen in the body is the main culprit for urogenital symptoms in menopause, officially known as the Genitourinary Syndrome of Menopause (GSM). Oestrogen is very protective for the intimate tissues, and without it, tissues can become weak, thin, less elastic and more prone to infection. Thankfully there are many ways to support health in this area today. It’s about finding out what’s right for each individual from a selection of options, including diet, medication, or lifestyle interventions.
Symptoms of peri-menopause
In the run-up to menopause, the period of peri-menopause, hormones fluctuate before they eventually decline. It's these fluctuations that cause many of the early symptoms of menopause such as hot flushes, disturbed sleep and changing emotional states. Vaginal symptoms may be experienced too, such as vaginal dryness, discharge and irritation.

Genitourinary Syndrome of Menopause
Common symptoms of the Genitourinary Syndrome of Menopause (GSM) include:
- Vaginal dryness & irritation
- Abnormal discharge
- Dyspareunia (painful sex)
- Decreased libido & sexual dysfunction
- Urinary urgency & frequency
- Increased incidence of UTIs

Vaginal probiotics
Recent studies show that probiotics containing Lactobacillus can help maintain vaginal and urinary tract health, reducing the incidence of UTIs even in the absence of oestrogen, such as in women on oestrogen-blocking therapy for breast cancer. By replenishing Lactobacilli, probiotics help prevent the colonisation of harmful bacteria like E. coli.
The vaginal and urinary microbiome are altered after menopause, with fewer healthy bacteria and more diverse bacteria capable of causing infections.
Lower levels of lactobacillus in the vagina and bladder can have significant health consequences.
- Menopause predisposes women to recurrent UTI (rUTI), due to lower levels of oestrogen leading to changes in the urogenital epithelium and subsequently urogenital microbiome.¹
- The risk of Bacterial Vaginosis (BV) increases with age and with previous BV diagnoses.²
- After menopause, oestrogen depletion elevates vaginal pH, reduces vaginal colonisation by lactic acid-producing microbes and facilitates colonisation by enteric organisms. This increases the risk of UTIs, a factor that contributes to incontinence in older women.³
- There is accumulating evidence for the role of the post-menopausal vaginal microbiome in endometrial cancer. A 2019 study identified postmenopausal status as the main driver of a polymicrobial network associated with endometrial cancer microbiome.⁴
We understand the science, and are equipped to help women overcome vaginal dysbiosis
Lactobacillus benefits:
- Lactic acid producing
- Maintain pH 3.7 - 4.5
- Produce bacteriocins, anti-microbial activity
- Adhere to cell walls, creating a barrier to pathogens
“Lactobacillus is a probiotic organism that can help prevent urinary tract infections (UTIs) by competing with pathogens, producing inhibitory substances, and modulating the immune response."5
Pathogens associated with:
- Increased levels of inflammatory cytokines
- Less healthy cervical mucus
- Increased immune activity
- Increased incidence of vaginal infections and urinary infections
“AV (aerobic vaginitis) results in severe inflammation and irritation. Common symptoms of this disease include sticky fishy odour, yellow discharge, and dyspareunia (painful intercourse)."6

Vaginal probiotics
Shop Pelvic Relief vaginal probiotics, formulated with clinically researched strains to restore balance, relieve bacterial imbalances and promote optimal urogenital health naturally.

Microbiome screening
Learn about our innovative Vaginal Microbiome Test and find the right options just for you.
REFERENCES: 1. Jung C, Brubaker L. The etiology and management of recurrent urinary tract infections in postmenopausal women. Climacteric. 2019 Jun;22(3):242-249. 2. Hoffmann JN, You HM, Hedberg EC, Jordan JA, McClintock MK. Prevalence of bacterial vaginosis and Candida among postmenopausal women in the United States. J Gerontol B Psychol Sci Soc Sci. 2014 Nov;69 Suppl 2(Suppl 2):S205-14. 3. Farage, M.A., Miller, K.W., Song, Y., Sobel, J. (2015). The Vaginal Microbiota in Menopause. In: Farage, M., Miller, K., Maibach, H. (eds) Textbook of Aging Skin. Springer, Berlin, Heidelberg. 4. Park MG, Cho S, Oh MM. Menopausal Changes in the Microbiome-A Review Focused on the Genitourinary Microbiome. Diagnostics (Basel). 2023 Mar 21;13(6):1193. 5. Reid G, Burton J. Use of Lactobacillus to prevent infection by pathogenic bacteria. Microbes Infect. 2002 Mar;4(3):319-24. 6. Mohankumar B, Shandil RK, Narayanan S, Krishnan UM. Vaginosis: Advances in new therapeutic development and microbiome restoration. Microb Pathog. 2022 Jul;168:105606.


